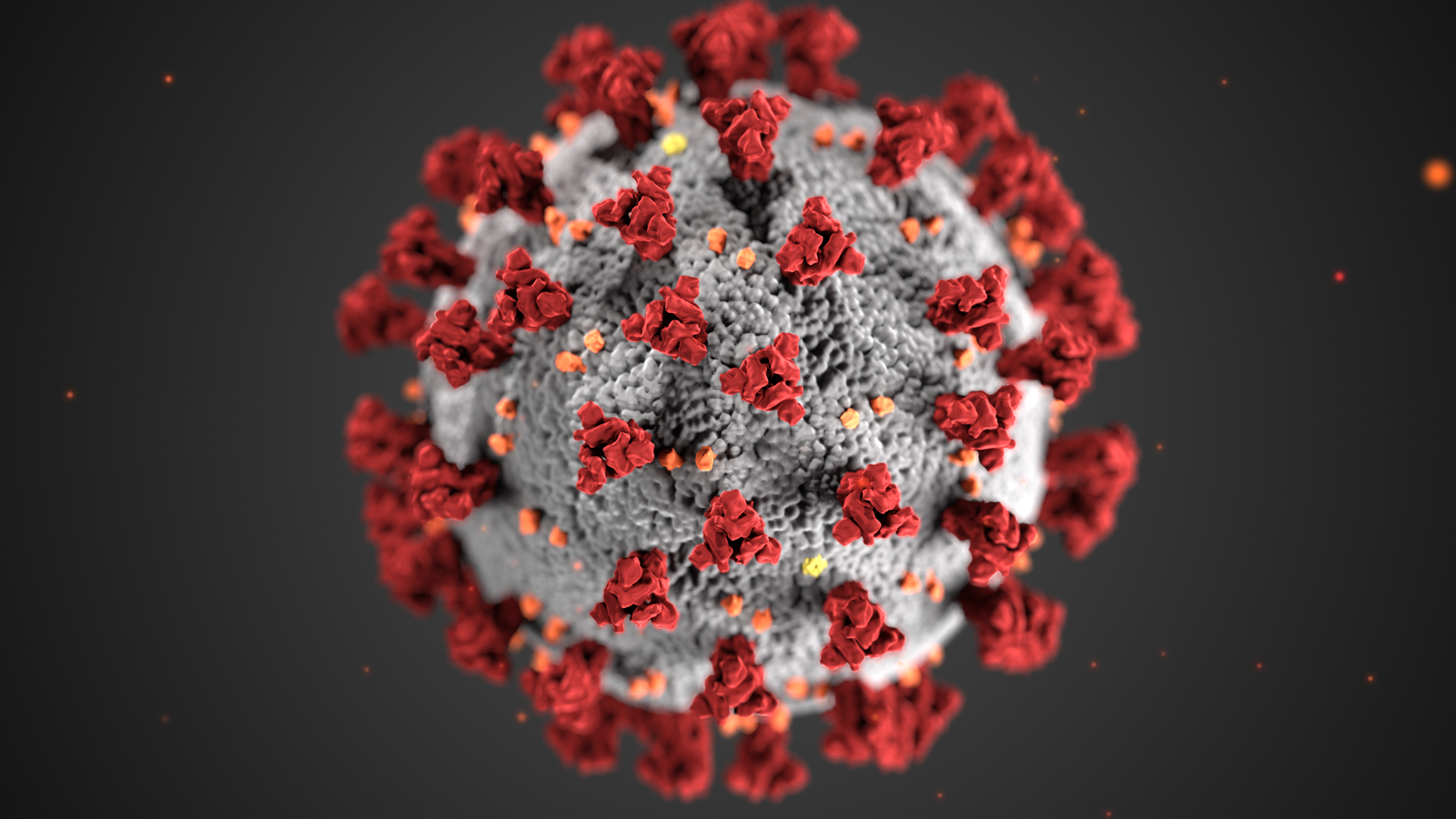
The New Year brought with it new mutants of the virus causing Covid-19. Subsequently, the world saw the arrival of the Delta-variant of SARS-CoV-2, which is a highly transmissible variant. It has mutated further to form the ‘Delta plus’ or ‘AY.1’ variant. Scientists said that there is no immediate cause for concern in India as its incidence in the country is still low.
The new Delta plus variant has been formed due to a mutation in the variant designated as Delta or B.1.617.2. Delta was first identified in India and was one of the drivers of the deadly second wave. There is no indication yet of the severity of the disease due to the new variant. But, Delta plus is resistant to the monoclonal antibody cocktail treatment (Casirivimab and Imdevimab) for Covid19 recently authorised in India.
Vinod Scaria is a clinician and scientist at Delhi’s CSIR-Institute of Genomics and Integrative Biology (IGIB). He tweeted on Sunday, “One of the emerging variants is B.1.617.2.1 also known as AY.1 characterized by the acquisition of K417N mutation.”
Scaria said that the mutation is in the spike protein of SARS-COV-2, which helps the virus enter and infect the human cells.
Also See: New mutants of Coronavirus
Under the global science initiative GISAID, 63 genomes of Delta (B.1.617.2) with the new K417N mutation have been identified so far, as per Public Health England.
In its latest report on coronavirus variants, updated till last Friday, the health agency said that Delta plus was present in six genomes from India as of June 7.
Mr Scaria further wrote on Twitter, “The variant frequency for K417N is not much in India at this point in time. The sequences are mostly from Europe, Asia and America.”
In late March this year, the earliest sequence of this genome was found in Europe.
Also Read: Indemnity from liability to be granted to vaccine manufacturers like Pfizer and Moderna
The travel histories for the variant are not readily available to make assumptions. Based on this input, Mr Scaria said that an important point to consider regarding K417N is the “evidence suggesting resistance to monoclonal antibodies Casirivimab and Imdevimab”.
The Casirivimab and Imdevimab combination recently received emergency-use authorization in India from the Central Drugs Standard Control Organisation. The antibody cocktail have been priced at a steep ₹ 59,750 per dose by the Drug majors Roche India and Cipla.
Antibodies are proteins that the body naturally produces to defend itself against the disease. Similar to them, monoclonal antibodies are artificially created in a lab and tailor-made to fight the disease that they treat.
Casirivimab and Imdevimab are monoclonal antibodies (MAB) that are specifically directed against the spike protein of SARS-CoV-2. These MABs are designed to block the virus’ attachment and entry into human cells.
The CSIR-IGIB scientist also indicated that the mutation may be associated with the ability to escape the immune response against the virus.
Immunologist Vineeta Bal noted that there may be some setback in the use of commercial antibody cocktail due to the new variant. Allaying fears, she added that resistance to the therapy is not an indication of higher virulence or severity of a disease.
Ms Bal is a guest faculty at the Indian Institute of Science Education and Research, Pune. She said, “How transmissible this new variant is will be a crucial factor to determine its rapid spread or otherwise.”
Neutralising antibodies are responsible for defending cells from pathogens. Ms Bal noted that the quality and quantity of such antibodies generated in the individual infected with the new variant is unlikely to be affected because of the mutation.
The immunologist faculty at IISER Pune said, “Thus, in individuals catching infection with the new variant, it may not be a matter worth worrying.”
On this point, Pulmonologist and medical researcher Anurag Agrawal, the director of CSIR-IGIB concurred. He said, “There is no cause of concern due to the new variant in India as of now.”
He also said that the blood plasma from many fully vaccinated individuals will have to be tested against this variant to determine whether it shows any significant immune escape.
Also Read: An unique Microchip unveiled by Pentagon- the chip can detect presence of Coronavirus in blood
Delta variant continues to evolve and acquire new mutations. Hence, there is a lot of interest in understanding its evolution. Director of CSIR-IGIB said that SARS-CoV-2 has a nearly constant rate of acquiring genetic variants. He also added that each variant has acquired additional variants in a stepwise fashion.
He further added, “Understanding this continued evolution is of great importance in mapping the evolutionary landscape of emerging variants. Largely, the virus has tried to optimise for transmission and immune escape by step-wise acquisition of new mutations.”
The formation of the Delta plus variant of the SARS-CoV-2 is a result of K417N mutation. This mutation of the spike protein causes the virus to enter and infect human cells.
Bani Jolly, a scientist who specialises in genomic sequencing, wrote about the new variant on Twitter, “A small number of sequences of Delta (B.1.617.2) having spike mutation K417N can be found on GISAID. As of today, these sequences have been identified in genomes from 10 countries.”
“The sequences have recently been designated as lineage AY.1 (B.1.617.2.1), a sub-lineage of Delta, due to concerns about K417N being one of the mutations found in the Beta variant (B.1.351),” Jolly further added.
Also Read: Does SARS-Cov-2 have any natural predecessor?
The presence of the Delta plus variant is still low in India. Therefore, scientists have not sounded the alarm. CSIR-IGIB scientist Vinod Scaria said, “The variant frequency for K417N is not much in India at this point in time. The sequences are mostly from Europe, Asia and America.”
The sequences have come from a number of countries across the world, other than India. The countries include USA, Canada, United Kingdom, Russia, Japan, Portugal, Poland, Turkey, Nepal and Switzerland, as per Outbreak Info.
Genomic sequencing specialist Bani Jolly said, “Looking at the large (T95I) cluster, it seems like AY.1 has arisen independently a number of times and could be more prevalent than observed in countries with limited genomic surveillance.”